The Key Role of Dr. Katalin Karikó in the Discovery of mRNA Vaccines
Author: Sandor Szabo, MD, PhD, MPH
Edited by: Christina Yoo, AA, BA, MA
American University of Health Sciences, School of Medicine,
Signal Hill/Long Beach, CA
A recent issue of The New England Journal of Medicine, the most widely read and famous weekly medical journal in the world, carries a front-page editorial on the “History of Medicine…” that covers not only the discovery of the COVID-19 mRNA vaccine, but in 2.5 pages, the entire history of the development of all vaccines.
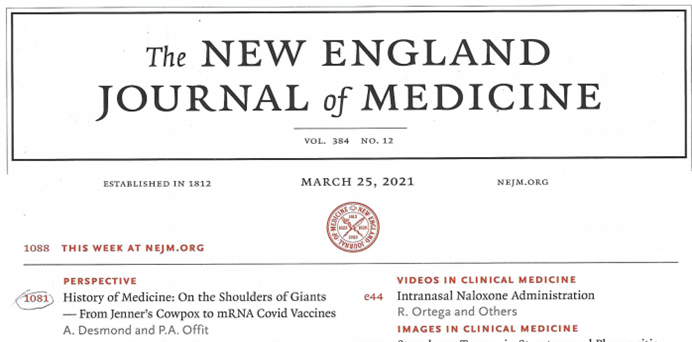
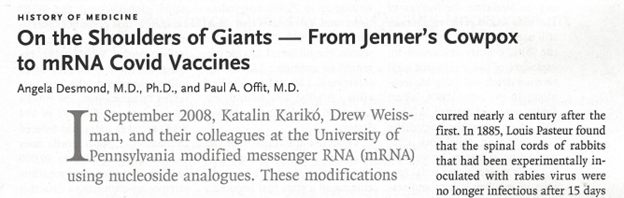
Thus, for historical reasons, all of us in the healthcare and education field should read this short review article. As you can see from the first line, it gives credit to the Hungarian scientist Katalin Karikó, PhD, whose collaboration with Drew Weisman, MD, PhD led to the development of the mRNA vaccine that forms the basis for the Pfizer and Moderna COVID-19 vaccines… Some of us deduced the seminal work of these two scientists still in December, as outlined in my public health update from Dec. 29, 2020.
- Why are the novel mRNA vaccines different from traditional vaccines? – All the antibacterial and antiviral vaccines developed so far are attenuated, weakened microbes that when injected into us, we produce antibodies which will recognize the dangerous viruses or bacteria when they enter our body, and kill or neutralize them. The creativity and originality of Dr. Kariko (who devoted her entire research career to developing mRNA-based therapeutics) has been that after last January when the genetic sequence of SARS CoV-2 has been published, along with electron microscopic pictures that the new virus attaches via its spikes to the ACE-2 receptors to animal or human cells, Dr. Kariko and other research teams focused only on the genetic sequence of spike proteins and their mRNA that encodes these proteins. Her reasoning has been that if we develop antibodies against the spikes, the virus cannot attach to our cells. In other words, by her reasoning: “Forget about the whole virus; let’s just concentrate our efforts to neutralize the spikes.” – and her ingenuity, along with technical help from Drew Weissman, MD, PhD from Boston, paid off and laid the foundation of BOTH current mRNA vaccine developments. Now, both will be nominated for the Nobel Prize.
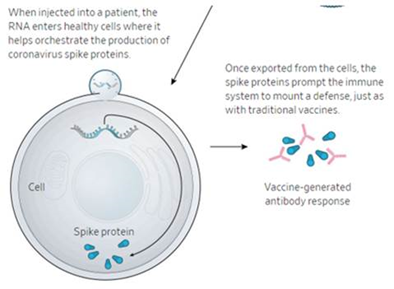
How mRNA vaccines work. – As you may surmise from the above description, these vaccines don’t use the entire attenuated virus, just the SARS CoV-2 spike protein-related mRNA. Strictly speaking, only the Pfizer vaccine uses the real mRNA; Oxford-AstraZeneca chose its double helix DNA analogue which makes this more stable (stored at -4 and not -80 ℃), as you will see later. The vaccines thus contain either mRNA or DNA that when entering our immune cells, they stimulate the production of spike protein and when they are released, other immune cells recognize this as “foreign” (not part of our body) and start producing antibodies against the spike proteins. The next step is predictable: when vaccinated persons catch the real virus, their bodies have millions of ready-to-attack specific antibodies to neutralize or kill the virus. This is shown in the illustration, below:

- What are the differences between the Pfizer-BioNTech & Oxford-AstraZeneca vaccines? – Two major differences:
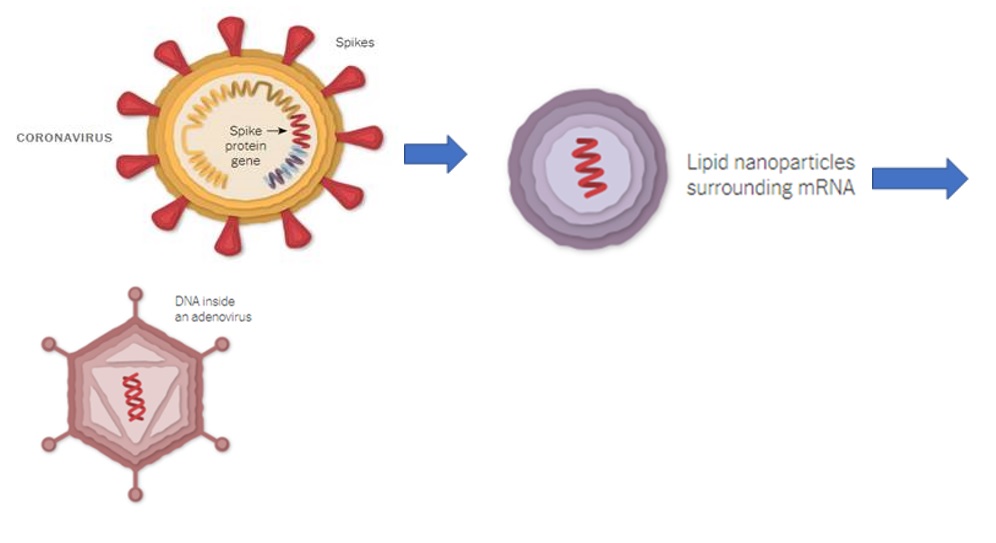
- As I mentioned above, the Pfizer vaccine contains the real mRNA of the COVID-19 virus, while the AstraZeneca applies the stable, related double helix DNA. The Moderna vaccine also uses mRNA, encapsulated in a thicker layer lipid in an oily micro-bubble – hence it’s more stable than the Pfizer variant. (https://www.nytimes.com/interactive/2020/health/moderna-covid-19-vaccine.html )
- Pfizer uses the unstable mRNA in an oily, protein microcapsule that also contains trace amounts of polyethylene or polypropylene glycol (PPG) to which some people are allergic. Hence the reported few cases of allergic reactions – but none of those were severe and life-threatening. The Oxford – AstraZeneca scientists placed the DNA into weak adenovirus (which in virulent form may cause pneumonia) that after, vaccine injections also taken up by our cells to produce spike proteins that, when released and recognized as ‘foreign’, our B-lymphocytes and plasma cells start producing massive quantities of specific anti-spike protein antibodies.
- Which vaccine is safer & which one should I take? – This is NOT a difficult question; both mRNA vaccines (Pfizer & Moderna) as well as the DNA-based (Oxford-AstraZeneca) variant are extremely safe and unbelievably effective (90-95%)! Compare this with the effectiveness of about 50% of our yearly flu (influenza) vaccines. Personally, I would take any of the 3, but if I had a choice, I would take the Pfizer or Moderna vaccines, since AstraZeneca employs the adenoviral vector delivery system. Namely, since my research lab used this technique in our first ever demonstration of curing/healing experimental duodenal ulcers in rats by a single shot of gene therapy (either naked DNA or adenoviral vector delivering angiogenic growth factors), we know that the weakened adenovirus might turn into an aggressive virus in the body and cause pneumonia both in experimental animals and patients, as the clinical literature demonstrated). [Deng XD, Szabo S, et. al… Gene therapy with naked DNA or adenoviral vector of VEGF or PDGF increases endogenous VEGF, PDGF and bFGF expression and accelerates chronic duodenal ulcer healing in rats. J. Pharmacol. Exp. Ther. 2004; 311:982-988.] Based on this date, of course, we could say that the Oxford-AstraZeneca vaccine is a form of gene therapy – applied early, to prevent diseases caused by new coronaviruses.
- Is the new mutation of SARS CoV-2 more dangerous? – Yes and no. Yes, it’s more infectious than previous variants (relax, more than 30 mutations have been demonstrated around the world), but we don’t know if the clinical outcome of these infections will be more severe than what we know so far from COVID-19 cases. Although the new mutations, which were first detected in the UK and South Africa, spread rapidly, are more transmissible, and apparently, are not deadlier. The other good news is (again, we know this from the often-disparaged basic science investigations) that mutations occur mostly in the base and middle, not at the tip of spike proteins that attach to our ACE-2 receptors. Thus, if the tip of spike proteins is not markedly altered, all the current COVID vaccines will be effective.