By: Sandor Szabo, MD, PhD, MPH
Professor, American University of Health Sciences, Signal Hill/Long Beach, CA
In medical/clinical terminology, diseases by onset and duration are usually categorized as acute, subacute, and chronic. Acute illnesses generally develop suddenly and last often only a few days. Subacute diseases usually last 5-14 days, while chronic conditions develop slowly and may worsen up to 3 months or longer.
The new infectious disease COVID-19 (coronavirus disease – 2019) caused by SARS-CoV-2 represents a challenge not only for treatment, but also by definition of its duration. Namely, as we learned in 2020, most of the COVID-19 patients who develop signs and symptoms of the disease (e.g., fever, fatigue, respiratory challenges) will eventually recover in about a week. During the last about 10 months, however, scientific reports appeared in medical literature describing many COVID-19 patients who developed long-lasting sequelae that are not only related to the respiratory tract but may involve almost any organ; most symptoms occurring in the central and peripheral nervous system. These conditions have been called long-hauler syndrome, or ‘post-acute disease’ or long-COVID-19, and the most preferred designation appears to be ‘long-COVID-19’. But since this is just not a simple disease like pneumonia or myocardial infarction or stroke, but a constellation of many waxing and waning symptoms, it is more appropriate to call this a syndrome, i.e., ‘Long COVID-19 Syndrome’ (LCS). In LCS fatigue, body aches, shortness of breath, difficulty concentrating, headache, and loss of taste or smell could persist for 4-8 weeks, after the initial, acute COVID-19, or if the patient recovered, these and other signs and symptoms may come back in 4-8 weeks. The neuropsychiatric signs and symptoms of LCS are probably the most prevalent and severe, and may include fatigue, myalgia, headache, cognitive impairment (‘brain fog’), while anxiety, depression, sleep disturbances, and PTSD occur in 30-40% of COVID-19 survivors. The pathophysiologic mechanisms of neuropsychiatric complications involve microvascular thrombosis, immune dysregulation, and inflammation. Other organ systems involved in LCS include the respiratory, cardiovascular, hematologic, gastroenterological, endocrine, and renal systems. The recently published report in the prestigious Lancet Psychiatry journal (May 2021) on the 6-month neurological and psychiatric outcomes in more than a quarter of million survivors of acute COVID-19 revealed dramatic increases in intracranial hemorrhage, stroke, dementia, and neuromuscular junction disorders that may explain, at least partly, the fatigues and weaknesses LCS patients experience:
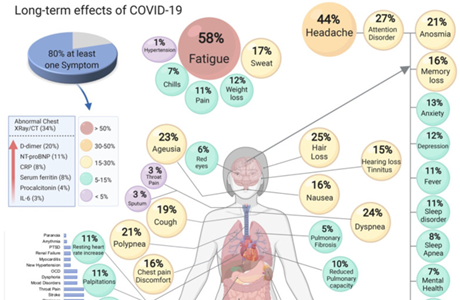
The long-term effects of COVID-19. (Adapted from: S. Lopez-Leon et al. More than 50 Long-term effects of COVID-19: a systematic review and meta-analysis. medRxiv 2021 Jan 30;2021.01.27.21250617)
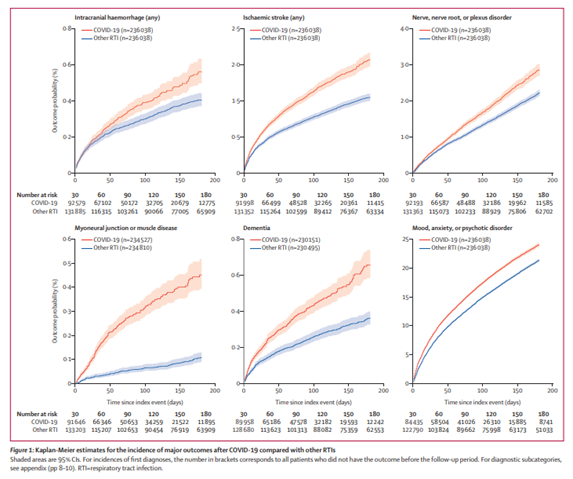
Major increases in neuropsychiatric diseases in ‘long COVID-19’ patients. (From: Taquet M et al. 6-month neurological and psychiatric outcomes in 236,379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry, 2021, 8, 416-427.)
Since LCS requires a lot more multidisciplinary investigations, especially from public health and preventive perspectives, we at AUHS, in collaboration with Drs. Pantelina Zourna Hargaden, Nils Lambrecht, John Schloss, and Deron Herr, applied for grants and initiated a large international collaborative study of ‘Long COVID-19’. The international collaborators are virtually all our formal colleagues, coworkers or students in 4 countries in Europe (e.g., Greece, Hungary, Germany, Ukranie), 2 countries in Africa (Ghana, South Africa), Malaysia and Mexico. The main goals of this 3-year prospective study is (1) to establish and compare the prevalence and incidence of new cases of LCS in these countries and USA; (2) identify potential nutritional deficiencies (e.g., zinc, selenium, niacin, thiamine) in LCS patients; (3) to find potential therapeutic and/or preventive measures for acute or chronic forms of COVID-19. This large international collaborative study is just another example of AUHS addressing local issues, but also reaching out globally.
June 11, 2021