Causes of Sudden Death
By Sandor Szabo, MD, PhD, MPH, AGAF, FRCPath.
Professor and Dean, School of Medicine
Physicians, especially pathologists like me, have been exposed to death many times, almost used to it (as many would say), but when this hits home, e.g., in the framework of ‘here and now’; we are also stunned… This recently happened to me on one Saturday in February: our best American friends (parents of my youngest son’s best friend from elementary and high school) invited us for a dinner and the event passed in excellent mood, and we all departed smiling, with plans for the next outing… Yet, Tuesday morning I got a phone call that Larry (67 years old, in perfect health, who had gone to a hot yoga class earlier that morning) had dropped dead at home, while his son saw him gasping for air, before bending over his desk, and becoming pulseless. His son called 911 and started CPR. The medical emergency team arrived in about 8 mins, started professional resuscitation, rushed him to the hospital, but Larry could not be revived, not even after electric shocks…
The shock in his and my family was associated with a puzzle: Larry was not only relatively young and very healthy, but living the healthiest lifestyle preventive medicine can provide, e.g., doing almost daily physical or yoga exercises, until a few years ago swimming in the ocean several miles/week, eating very healthy food, taking multivitamins and controlling his blood pressure – yet he succumbed to sudden death… Since his family didn’t want an autopsy performed that would have established or narrowed down the cause of his death, in subsequent days, I reviewed for his family the likely causes of a sudden death:
The most frequent causes of sudden death are cardiac or pulmonary in origin (stroke is often implied improperly):
- Myocardial infarction (MI) is a frequent etiology. This is due to a thrombus (blood clot), usually formed on the top ruptured atherosclerotic plaque in the left coronary artery (LAD) blocking the blood supply to the left ventricle of the heart. Lack of oxygenated blood means ischemic necrosis (cell death) in the most hard-working part of the heart and necrotic cardiac wall cannot push out the oxygenated blood through the aorta to other parts of the body. MI is usually associated with sudden, excruciating pain in the left chest, often irradiating to the left arm or chin (mandible). LAD is often narrowed by expanding atherosclerosis that is, unfortunately, progressing with our age. Hence the importance of healthy diet and taking statins, (Lipitor-like drugs) is critical for all of us, especially if this is associated with mini (‘baby’) doses aspirin (81 mg) that reduces the risk of thrombus formation, in addition to other health benefits like anticancer effects. Since aspirin often damages the gastric mucosa, especially in full doses (325 mg tablets), it is advisable to take enteric coated mini aspirin tablets or the new gastro-safe (Vazalore) 81 mg version.
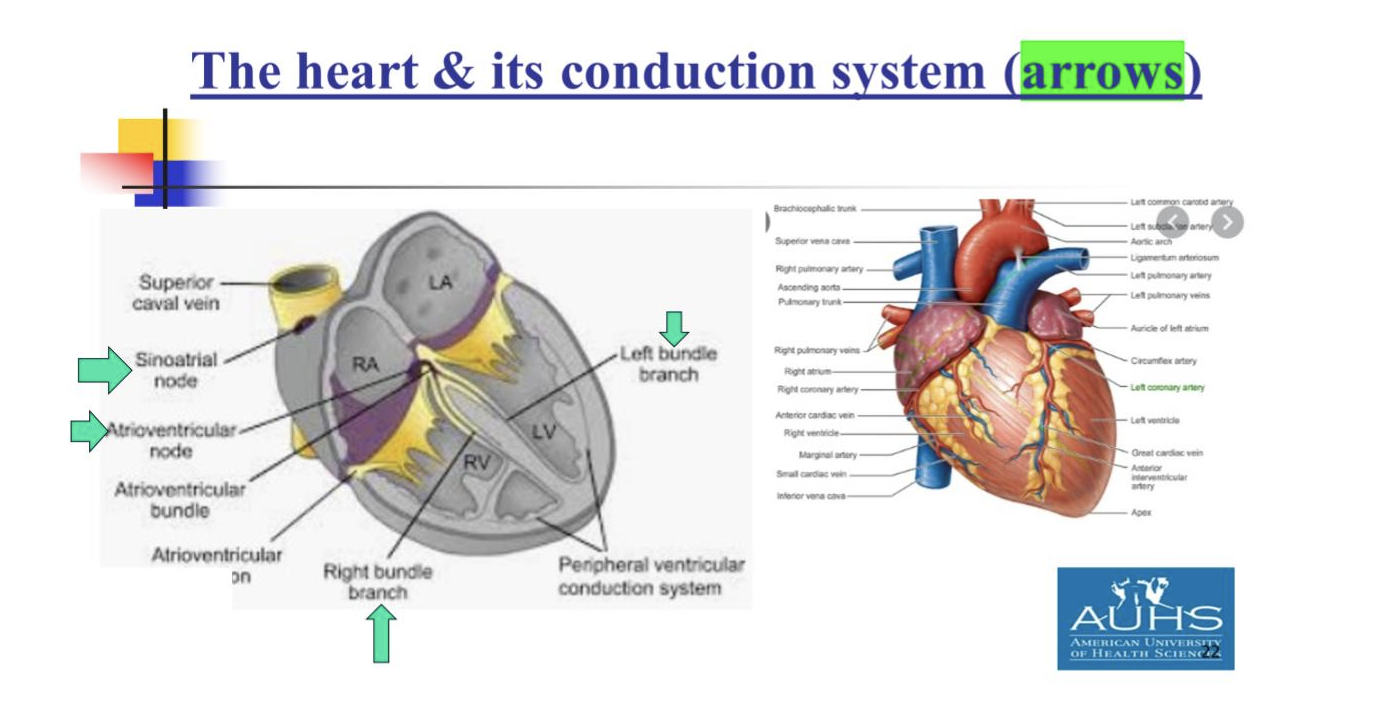
- Cardiac arrhythmias (CA) may occur suddenly, without any advance sign or symptoms and people may just collapse and die on the spot. This is the cardiac emergency when cardiac defibrillators may be lifesaving, since they may restore the normal rhythm (pulse) of the heart to about 70 bits/min. Namely, our hearts are programmed to about 70 contractions per minute, due to a small group highly specialized cardiac myocardial cells in the so-called cardiac conduction system, consisting of a sinus node (about 0.5 cm) in the wall of right atrium of the heart and atrioventricular (AVN), also about 5 – 8 mm, in the juncture of right atrium and ventricle. Although CA may strike at almost any age (e.g., we often hear and read about young athletes ‘dropping dead’ in the field), but here advanced age is also a predisposing factor. After performing or supervising more than 1000 autopsies in Boston and Long Beach, I noticed that as we age, the highly specialized cells in the conduction system are slowly being replaced by connective tissue – hence the number of rhythm-producing myocytes is gradually decreasing. Predisposing factors to CA are also well-known, since fatal CA is described in the literature after major psychologic distress (e.g., during or after major arguments in the family, or during the ‘broken heart’ syndrome after unexpected breakup with loved ones).
- Pulmonary embolism (PE) is often the unrecognized etiology of sudden death. This usually occurs when we sit idle for several hours (e.g., long-haul flights) or at a desk without any movement of our legs. These conditions slow down the venous blood flow from our lower extremities to the right side of the heart, predisposing the dilated veins to thrombus formation and if these thrombi are dislodged by the blood flow, they become emboli. If small, these emboli cause chest discomfort, cough, often difficulties in breathings, but if large (e.g., about 1 cm in diameter and 2-3 cm long – unfortunately, I have seen this in many of my autopsies) they completely block the blood flow to the lungs, resulting in immediate death. Analyzing the signs and symptoms of our friend Larry (e.g., gasping for air, no pain or preceding signs); PE was the most likely cause of his demise, likely combined with CA that could not be restored by defibrillation. Namely, if the heart does not get enough blood supply through the lungs, it goes into ‘over-drive’, often triggering fatal CA. Prevention of PE is similar to that of MI: statins, mini aspirin and frequent leg movements.
- Ischemic stroke is often associated with sudden death, but mortality is never as sudden and rapidly developing as with the previously described three cardiopulmonary events. These strokes are due to local thrombi (as in LAD leading to MI), but more frequently to emboli (e.g., from fibrillation of the left atrium) that obstruct blood flow to certain areas of the brain. If the ischemic area involves the brain cortex, it may cause leg or hand paralysis or loss of speech, but if the emboli block blood supply to the brainstem (where our respiratory and cardiac centers are located), the death is more imminent.
These cardiovascular complications indeed my cause sudden death, but some of these conditions are preventable. Thus, let’s practice prevention, as much as we can, and hope for good outcome.
References:
Robbins & Cotran Pathologic Basis of Disease. 9th ed., Elsevier Saunders, Philadelphia, 2015.
Mittleman R, Szabo S, Heinsimar J, Reynolds ES, von Lichtenberg F. Macroscopic histochemical detection of myocardial necrosis in the heart at autopsy by the triphenyl tetrazolium chloride (TTC) technique. Clin. Res. 1975; 23:198A.
Szabo S, Gerzic Z, Dugalic D. Lecenje srcanog zastoja (Treatment of cardiac arrest). Medicinski Podmladak 1968/69; 20:57-67.
Szabo S, Yoshida M, Filakovszky J, Juhasz Gy. “Stress” is 80 years old: From Hans Selye original paper in 1936 to recent advances in GI ulceration. Curr. Pharm. Des. 2017; 23:4029-4041.
March 26, 2024